LITERATURE - 2020, Journal of Hungarian Obstetricians and Gynaecologists
Hematohydro-hysterocolpos with vaginal atresia
Case report

Authors: Gherai Rareș1, Chitulea Petru2
1Department of Obstetrics and Gynaecology, Faculty of Medicine and Pharmacy, University of Oradea, Oradea, Romania
2Department of Obstetrics and Gynaecology, Faculty of Medicine and Pharmacy, University of Oradea, Oradea, Romania
Hydrocolpos is a rare condition, clinically obvious at birth, or within the first few weeks of life and it appears as an abdominal mass associated with the absence or abnormality of the vaginal opening. A premature 25 days old female new-born was diagnosed with hematohydrohysterocolpos, imperforate hymen. After the surgery, the evolution is positive and the patient is released from the hospital in a good general state.
Keywords: hymen, vagina, atresia, hematohydrohysterocolpos
Introduction
Hymenal anomalies result from incomplete degeneration of the central portion of the hymen. Variations include imperforate, micro-perforate, septate, and cribriform hymens. Although most of these variants are not clinically significant, hymeneal anomalies require surgical correction if they block vaginal secretions or menstrual fluid, interfere with intercourse, or prevent treatment of a vaginal disorder.
Imperforate hymen represents a persistent portion of the urogenital membrane. It occurs when the mesoderm of the primitive streak abnormally invades the urogenital portion of the cloacal membrane. It is one of the most common obstructive lesions of the female genital tract. When mucocolpos develops from accumulation of vaginal secretions behind the hymen, the membrane is seen as a shiny, thin bulge. The distended vagina forms a large mass that may interfere with urination and at times may be mistaken for an abdominal tumour. Topical anaesthetic is used to prevent discomfort to the new-born, and the central portion of the obstructing membrane is excised. When imperforate hymen is corrected in infants, the central portion of the membrane is excised; sutures usually are not necessary.
If missed during the newborn period, imperforate hymen often is not diagnosed until an adolescent presents with complaints of primary amenorrhea and cyclic pelvic pain. It may present as back pain or difficulty with defecation or urination secondary to mass effect from vaginal distention. Inspection of the vulva may reveal a purplish-red hymenal membrane bulging outward as a result of accumulation of blood above it (hematocolpos). Blood may fill the uterus (hematometra) and spill through the fallopian tubes into the peritoneal cavity. Endometriosis and vaginal adenosis are known but not inevitable complications. Repair of imperforate hymen is facilitated if the tissue has undergone estrogen stimulation and the membrane is distended. When the procedure is performed in an adolescent, a large central portion of the membrane should be removed because the edges of a small incision may coalesce, allowing the obstructing membrane to reform. Hydrocolpos is an anomaly and a rare condition which occurs in new-born female infants as the result of the stimulation of maternal oestrogens; it consists of atresia of the vaginal outlet and excessive secretion of the cervical glands and produces a midline mass and building at the introitus. Regarding the aetiology, we find two theories in the academic literature, both of which may be regarded as correct:
- an imperforate hymen, which is the true cause;
- a thick membrane is responsible for it (considered to represent an atresia, similar to that of imperforate anus). Hydrocolpos is clinically evident at birth, or within the first few weeks of life, and it appears as an abdominal mass associated with absence or abnormality of the vaginal opening. The diagnosis is confirmed by abdominal ultrasound and CT scan.
Case Report
A premature new-born female, 25 days old, is admitted in the paediatric unit for the bio-clinical re-evaluation and a specialised treatment, having previously been diagnosed with congenital pelvic tumour. The medical history of the illness reveals that starting from the intrauterine life, affirmative, a tumour mass is being observed via ultrasound – approximately 5 cm in diameter, situated in the abdominal cavity, right next to the uterus, interpreted as a cystic ovarian tumor by the obstetrician. Postnatally, the new-born presents a good general state, with a balanced respiratory and cardiovascular function, present bowel transit and present diuresis. At the ultrasound checkup, the presence of a tumour mass in the intra-abdominal cavity is confirmed, having a mixed parenchymatous-fluid aspect, hard to appreciate as being part of the organ. In order to identify the nature and the origin of this mass, a CT scan is being performed that shows images suggesting a cystic pelvic-subperitoneal mass. It is important to mention that the examinations conducted in the laboratory have not highlighted any alterations of the renal function.
The general clinical examination reveals a voluminous distended abdomen which highlights a tumour mass in the hypogastrium with the palpation of a firm mass, adherent to the subjacent plans, painless, unique, of 6/7 cm dimension (Photo 1)..

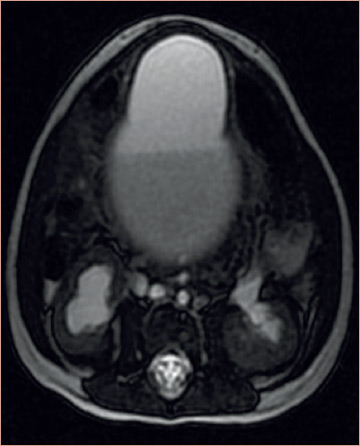
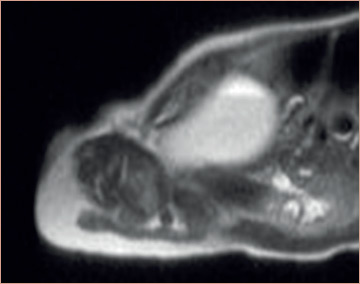
The abdominal ultrasound highlights a space occupying abdominal-pelvic process, with fluid content, a possibility of an increased volume of the uterus, with difficult limits to set, with hematocolpos and bilateral hydro nephrosis with secondary compression. A specialised team, comprised of a surgeon and an oncologist, decide the timing of the procedure in order to precisely establish the affected organ through MRI studies. The images provided by the MRI advocate for a giant fluid abdominal-pelvic mass with (most probably) uterine connections and secondarily bilateral hydro nephrosis (Figure 1–3).
The laboratory examination revealed the changes: increased levels of Lactate dehydrogenase (LDH) – 267 u/L, AFP alpha-fetoprotein 486.64 ng/mL, total serum proteins 5.35 g/dl, serum creatinine 0.20 mg/dl and a decrease in urea nitrogen 9.27 mg/dL.
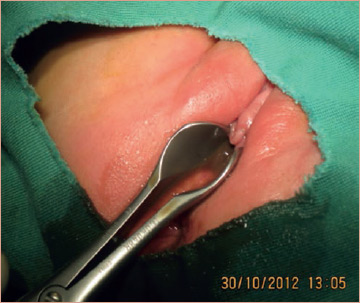
As a result of these investigations, clinical and paraclinical, after the gynaecological examination which highlights the imperforate hymen, we set the diagnosis of hematohydrohysterocolpos, imperforate hymen and after a thorough preoperative preparation, we performed the surgery. A No 18 needle was inserted into the membrane at the introitus, and 20 ml of haematic, brownish liquid was removed, when we observed a vaginal atresia. Then, on needle path, we performed a straight and deepness incision of approximately 1 cm at the introitus membrane, at a distance from the urethra, bladder and the rectum in order to not sever them. On the colpos incision, we evacuated about 200 ml of haematic, brownish liquid. At the end, a drainage tube was fixed through the incision in order to ensure the complete evacuation of the intraperitoneal content, which was removed after 7 days (Photo 2–4).
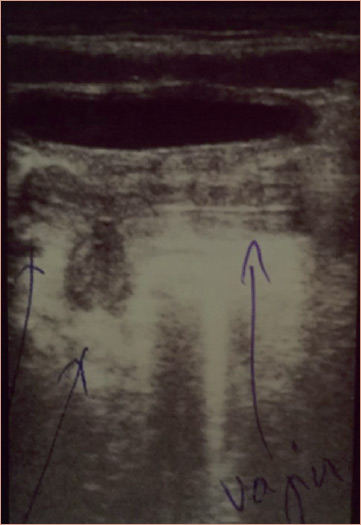
The follow-up abdominal ultrasound performed (Figure 4) in the first day after the surgery highlights an decreased of the bilateral hydro nephrosis from stage II, prior to the surgery, to stage I – a uterus significantly reduced in size, without any fluid in it. Under antibiotic cover the evolution is positive and the patient is released from the hospital in a good general state 10 days after surgery. After this, the child is being periodically followed up to monitor normal subsequent development of the genitalia (Figure 5).




Conclusion
Females with vaginal atresia lack the lower portion of the vagina, but otherwise have normal external genitalia. The embryonic origin of this condition is presumed to involve failure of the urogenital sinus to contribute its expected caudal portion of the vagina (Simpson, 1999). As a result, the lower portion of the vagina, usually one fifth to one third of the total length, is replaced by 2 to 3 cm of fibrous tissue. In some individuals, however, vaginal atresia may extend to near the cervix.
Since most women with vaginal atresia have normal external genitalia and upper reproductive tract organs, this condition does not often become apparent until the time of expected menarche. Adolescents generally present shortly after physiologic menarche with cyclic pelvic pain due to hematocolpos or hematometra. On physical examination, normal breast and pubic hair development is present. The perineum is usually normal, with normal secondary sex characteristics with a hymeneal ring and beyond the ring, a vaginal dimple or small pouch. A recto-abdominal examination confirms the presence of midline structures. Additionally, sonographic or MR imaging will display upper reproductive tract organs. Of these, MR imaging is a more accurate diagnostic tool, as the length of the atresia, the amount of upper vaginal dilatation, and the presence or absence of a cervix can be identified. Laparoscopy, however, is necessary for diagnosis when the anatomy cannot be fully evaluated with radiographic studies. For example, Economy and associates (1998) reported that MR imaging has only 31-percent sensitivity for the detection of uterine structures in patients with vaginal agenesis. About one third of women with vaginal atresia have associated urologic abnormalities. Vaginal atresia is distinct in clinical and embryonic characteristics from transverse vaginal septum. In patients with transverse vaginal septum there is a well-developed vagina in which a thick intervening septum separates the lower from the upper vagina. Conversely, in those with vaginal atresia, fibrous tissue develops in place of the vagina. In some, nearly the entire span beginning at the perineum and extending cephalad to the cervix may be fibrotic. Identification of the cervix in such cases distinguishes vaginal atresia from mullerian agenesis. The imperforate hymen and/or atresia of the distal vagina can be caused by fluid and blood successive to the genital crisis of the new born baby so that the hematohydrohysterocolpos to produce pseudo cystic pelvic tumours susceptible to compress both ureters leading to hydronephrosis. The advisable/opportune surgical treatment that involves the evacuation has, including, the foetal vital indication.
Conflict of interest
The authors declare no conflict of interest.
References
- Adaletli I, Ozer H, Kurugoglu S, et al. Congenital imperforate hymen with hydrocolpos diagnosed using prenatal MRI. AJR Am J Roentgenol 2007; 189(1): W23.
- Decherney AH, et al. CURRENT Diagnosis & Treatment Obstetrics & Gynecology, Tenth Edition; 2012 Sept., Cp.34.v
- Lim YH, Ng SP, Jamil MA. Imperforate hymen: report of an unusual familial occurrence. J Obstet Gynaecol Res 2003; 29: 399. [PMID: 14641689]
- Pitkin J, et al. Obstetrics and Gynaecology. Developmental and paediatric gynaecology 2003; p. 89.
- Plumb RT, Kelly JR, Dillon JR. Hydrocolpos in a Newborn Child. Western Journal of Medicine 1963 Oct; 99(4): 263–265.
- Schorge, et al. Section 2 Reproductive Endocrinology, Infertility, and the Menopause > Chapter 18. Anatomic Disorders – Vaginal agenesis, Williams Gynecology 1 edition, April 2008.
- Sidatt M1, Ould Sidi Mohamed Wedih A, Ould Boubaccar A, Ould Ely Litime A, Feil A, Ould Moussa A. Hydrocolpos and hydrometrocolpos in newborns. PubMed 2013 Feb; 20(2): 176–80.
Download Full Article
- Gherai Rareș: Hematohydrohysterocolpos with vaginal atresia (2020, Journal of Hungarian Obstetricians and Gynaecologists, PDF, 4 pages, English, 879KB)